5 Minute Read
This is a first. To our knowledge no systematic effort to account for the number of practices providing integrated behavioral health services in the United States has been undertaken, other than efforts to identify colocated providers in a geographical space. To be sure the data collected has its limitations and this blog is not peer-reviewed, however, the data is an illuminating start to what we hope is a more comprehensive picture of efforts to break down the silos within the healthcare delivery system. Here is what we at the Collaborative Family Healthcare Association (CFHA) learned in our first year of collecting data on sites providing integrated care services. (And if you are new to integrated care, check this summary out.)
The Big Picture
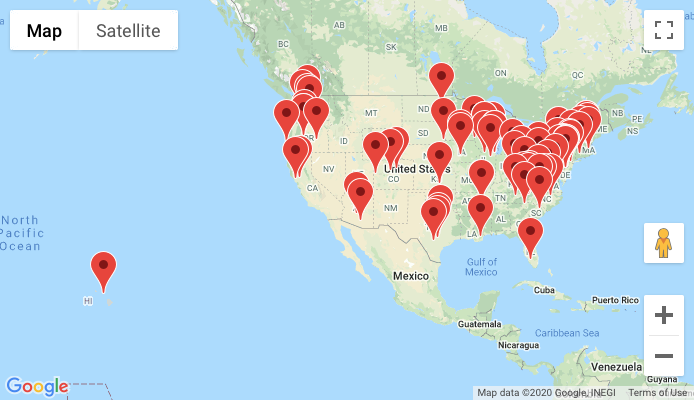
The data portray a complex reality of combinations of service types being offered to all or some of a clinic’s population. In short clinics appear to be finding it necessary to combine models and service types in order to meet patient needs. Most clinics offered more than one kind of integrated service. This could be due to more than half of the clinics providing services to underserved populations. The data also show a spread of integrated care across the United States and demonstrate how many lives are potentially affected by this spread. Assuming the likelihood that we have not captured even the majority of sites in the United States providing these services, the collective impact is significant, numbering in millions of lives annually. Missing data is also an important aspect of the picture below. Clearly the data below would change if other systems of care were more represented, like the Department of Defense, Veteran’s Administration clinics and private/ commercial health systems. There are also a good number of states with missing data. Additionally the sites represented are primarily primary care sites and we know that integrated care efforts are underway across the health system. So, there is work to do to fill in the picture, but the numbers are encouraging and give us a place to start the conversation about how widespread integrated care is at present.
The Data
80 Organizations who reported data
30 Number of states with integrated care organizations
504 Estimated total locations where patients could find integrated care services
2,260,000 to 4,860,000 Estimate range of patients with access to integrated care services
57.5% Sites identifying as either FQHC, RHC, CHC or academic safety net clinic
Breakdown of service types provided (as a percentage of all clinics reporting access for some or all patients in their population):
Primary Care Behavioral Health Model: 88.8%
Collaborative Care Model: 57.5%
SBIRT: 70.0%
Medication Assisted Treatment: 66.3%
Specialty Therapy: 58.8%
Medical Family Therapy: 21.3%
Specialty Addictions: 40%
Bidirectional: 28.8%
Specialty Psychiatry: 38.8%
Consulting Psychiatry (general): 57.5%
Telehealth (pre-pandemic, for mental health): 50%
What This Tells Us
The clinics reporting data are likely high performing clinics and as such may not be representative of all clinics providing integrated care services. That said, the impact of even 80 clinics providing these services on patient access to integrated care is substantial. The diversity of services offered is also a telling indication of what happens when models are dropped into healthcare ecosystems – clearly evolution takes over and unique solutions reign. This may be a telling indicator for researchers and model proponents to plan for this phenomenon and consider contextualizing their study efforts in real-world settings where a diversity of integrated care efforts exist. And although financial sustainability data is not captured in our map, the spread of integrated care demonstrates that somehow systems and clinics are making this work, even without substantial payment reform across the health system. At the very least in the case of the majority of the clinics reporting data, this may also be an indication that the investment of the department of Human Resources & Services Administration (HRSA) & Substance Abuse & Mental Health Services Administration (SAMHSA) has had tangible results.
What We Need
So, this is a good start, but only a start. We need enterprising researchers to do more to enumerate the spread of integrated care, the impact of this care and detail the contexts in which care is being transformed. Consider this blog post a nudge in that direction. Additionally we will need to assess the impact of the pandemic on these services. Anecdotally services appear to be even more highly utilized than pre-pandemic and the number of sites providing telehealth services is nearly 100%. Those changes only reinforce the need for integrated care, but we need more information on what those changes mean for the teams providing care.
We will do our part to continue to fill in the map and keep it updated. If you are interesting in submitting data, we make it easy to do so here.

If you want to grow your know-how just keep visiting this site and be updated with the most up-to-date news update posted here. Francisca Neddy Filberte